Who doesn't want to make managing their health and health care easier? But changing unhealthy habits and navigating the fragmented health care system can be challenging at best.
Aetna-CVS, the largest health company in the US, is shaking things up. It also happens to be run by the woman at the top of Fortune's Most Powerful Women of 2021 list, Karen Lynch, who stepped into her role just last February during the pandemic.
Lynch has put forward a bold vision that leverages her company's vast reach. The plan includes transforming hundreds of CVS drugstores into health "super clinics" that offer primary care services and mental health counseling in addition to prescription refills and over-the-counter sales. It's clear that Aetna-CVS is also leveraging data and analytics at every step of the way.
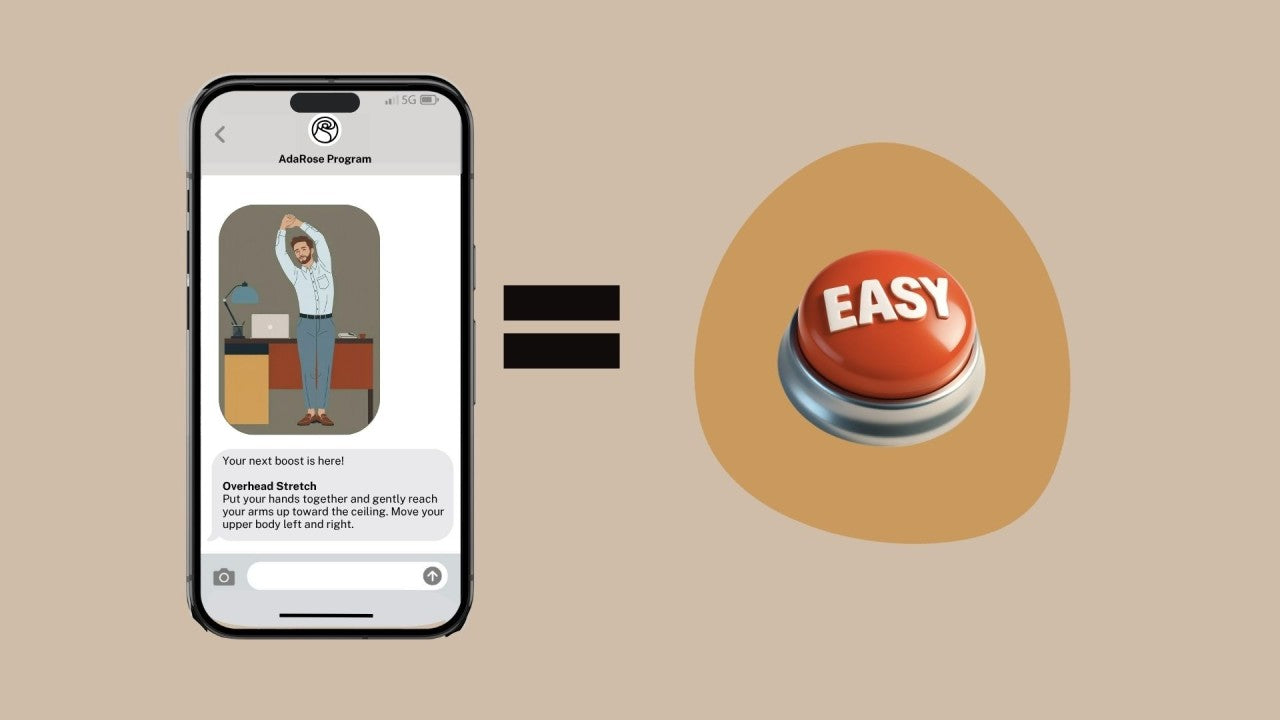
In this video, Rahul Kak, who was recently promoted to VP of Customer Health and Experience at Aetna-CVS joins Lygeia of AdaRose to discuss how the company is using data, analytics, and artificial intelligence (AI) to help its members achieve better health in a more seamless way.
Even if you aren't a member of Aetna or don't shop at a CVS (though 80% of Americans are within 10 miles of one) the way Aetna-CVS is holistically approaching customer care and leveraging technology will undoubtedly have implications for the rest of the country. So check it out and see what's in store for you and your family.
Interview Transcript
Lygeia:
Hello and welcome to the AdaRose digital health and wellness video podcast. I'm your host, Lygeia Ricciardi and our guest today is Rahul Kak. He is the Executive Director of Behavior Change Marketing at Aetna. Welcome Rahul! We're totally excited to have you.
So, some background before we jump into questions with Rahul. Aetna, your employer merged with CVS a couple of years ago. The combined entity is the single largest healthcare entity in the U.S. You provide benefits that cover about 40 million Americans. And some of these insurance plans are private, like employer plans, others are public, more like Medicare and Medicaid.
And I'm pretty sure that we have a number of Aetna customers listening. I am one of them. Happy to be one of them. I've been a member for a number of years. But even if you personally are not an Aetna member, what Rahul is going to tell us about is relevant to you because the kinds of changes that they're making and how they're using behavior change modification really has ramifications for all of us.
So again, whether you're getting [insurance] directly through Aetna right now or whether your plan is one of the many who's watching what Aetna does, the ideas that he talks about today are going to have an impact on you and your family at some time in the near future.
Welcome Rahul. We're very excited to have you.
Rahul:
Nice to be on this. Thank you. It's a pleasure to meet you, Lygeia, and be on your program.
Who is Rahul Kak and what does his role as Executive Director of Behavior Change Marketing mean? (1:31)
Lygeia:
Fabulous. So, given this context of Aetna, can you tell us a little bit about your specific role and what your title, Executive Director of Behavior Change Marketing really means? [Note: Rahul was recently promoted to VP, Customer Health and Experience at Aetna-CVS.]
Rahul:
Yes. It's not a common title you see at a lot of companies but one familiar way it's been described in other settings has been more on population health management. And that's the common way I usually describe what the work I do is.
So this is basically using marketing channels and other digital channels to proactively nudge people on their path to better health. And so this is going to come in the context of educational content and mailers, digital media, phone outreach, pharmacist discussions. And we can talk more about that, but in our case it's oftentimes powered by predictive learning models.
And a bit more detail on what we mean by "population health management." It's actually not just educating people about how to manage their own personal health, which I might traditionally classify as a category called "wellness." So what we're doing is guiding people on how they should be or could be interacting with their healthcare system, which is a lot more complex.
And that will be things like, where do I go for care? Am I getting the right treatments to manage my chronic conditions? Then ultimately, what should I talk to my doctor about?
Nudging consumers to make healthier behavior change decisions and navigating the healthcare system (2:56)
Lygeia:
So, with that kind of dual purpose, I would love to dig into a little bit more of the specifics in each area. So for example, on the wellness side, what might be some examples of the kinds of behavior that you can help to nudge people with
Rahul:
Yeah. And when I say "wellness," so wellness would be like mind and body, how do you manage it better? Usually these are things you can do on your own without interacting with the health system necessarily. So wellness would be things like eating right, sleeping early, or in a consistent way, or exercising frequently.
Now, when we talk about the focus of my group, which is on this more population health management and interacting with the healthcare system, it will be, I'm going to give you some specific examples now. So, it could be navigating folks to primary care locations or nearby urgent care options instead of using an expensive ER for unnecessary categories of care was a very specific example and like a very common one that any insurance company and providers are thinking about.
Other examples would be, how do you educate people to get certain preventative screenings like a mammogram or colon cancer testing? And then you can get more clinical in nature where it could be, what should you talk to your doctor about? Maybe considering adding a certain specialist to their care team or adding a specific type of drug to your regimen, because maybe we're predicting you to be at higher risk for a certain chronic condition.
So it becomes like a very expansive category that can also get very condition-specific, and it could be either predictive or deterministic based on exactly what kind of diagnoses you have.
Lygeia:
Yeah. You gave the population health analogy, and I know that many consumers may not be as familiar with that as folks in the healthcare world. But sort of in brief, I think in part, just to clarify that for folks, that's partly about being able to look across the population and say, hey, we should really be focusing on these people because they're at risk of something relative to others.
What might be an example of how that would work? So again, I mentioned I'm an Aetna member personally. Let's say I, let's get a real life scenario. I want to get a COVID shot. Or maybe you don't even know that yet, but you might assume that I do because of where we are in the pandemic and all.
So how might you use predictive analytics to maybe drop in and even figure out, I guess you would know whether I've had a shot or not because it would have gone through billing. Do you use that information?
How health insurers can better support their members through population health management (5:41)
Rahul:
Yeah, you can. So, I kind of casually dropped the terms like "deterministic" and "predictive." So let me break that down and to answer your question. I think there's probably a targeting component, and then the educational component, which will be like using channels to reach out to people.
So on the targeting component, we could do simple stuff where it's deterministic. We know, for example, as a health plan, what prescriptions you're on or past diagnosis codes or pre-certs on a procedure, and we could use this to think, okay, what's the next best action based on this specific thing we know with a 100% certainty this person has gotten or is managing?
And then there's a category of more predictive which is to say, we think statistically there's a high probability of determining that you are likely to need certain kinds of care, and then we're going to trigger a message to send to you. And so this is where data science is coming in: they're building machine learning models and training them with big data, all of these data points that sort of surround the history of this person's health behavior, consumer behavior, social determinants of health, engagement with certain channels.
And we'll use these past data points to predict the most relevant message at the best time or best pace. And this is, it's scientific but it's not perfect. So you have to be sort of thoughtful about, as a marketer, you have to be really thoughtful about messaging and acknowledging that you're not going to get it right all of the time. But we're doing this sort of in the best interest of what we think may be relevant for you. And then I can sort of talk about the channels.
What are the communication channels available to reach consumers to encourage healthier behaviors? (7:20)
Lygeia:
Yeah, no, I'd love to ask you about the channels actually, specifically. So you want to target somebody, what kinds of channels do you have at your disposal
Rahul:
Yeah. And the most traditional example that is probably undoubtedly the best way to help someone manage care, is to just have a live person. And many insurance companies do this, and managed care organizations do this, providers will do this where they'll have a care management staff, and it could be nurses or some sort of clinician.
They don't have to be clinical in nature, they could be some sort of case manager. But someone who can help walk you through your healthcare journey and make sure you.. simple things, maybe talk to you and encourage you to see a coach to make sure you're adhering to drugs and following the directions provided by your doctor.
And so, that is sort of the ultimate thing. But it's not scalable. So where my group comes in is, we're trying to supplement what I just described. And we're sort of adding scalability through different types of channels in automated journeys.
So then the channels we can think about, direct mail, email, text messages, there's phone calls, and that can be both live, say, with a care manager or automated phone calls, there's mobile app notifications, personalized micro-sites, paid digital media. We have an Apple watch program.
And I think sort of a crowning achievement in this sort of portfolio would be activating pharmacists. And so for my company for example, we have a footprint of 10,000 pharmacies, and then we have an ecosystem of minute clinics and health hubs.
And so, those are other tactics we can use if we're sending a message to a pharmacist, that can help reinforce certain recommendations that we can share if someone is in that setting. And really any of these settings I mentioned.
Real life application of using artificial intelligence to reach health plan members effectively (9:24)
Lygeia:
So that's a super-cool way to take advantage of this integration essentially between the role as insurer and the CVS piece. So again, just thinking in totally practical terms, so interestingly enough, so I am an Aetna member and I do often go to CVS. So let's say I go to CVS. Maybe I am taking an antibiotic for a particular infection that I have.
So you guys, your group would be able to ensure that essentially somewhat basic contextual information about me goes and is there sort of like a flag for the pharmacist to like, hey, this person's an Aetna member, while she's here you should probably talk to her about getting a flu shot or whatever else?
Rahul:
That's exactly right. You basically nailed it. There's a system in place where we can empower our pharmacists, and our pharmacy techs, to deliver certain types of messages that are relevant for them if there's a match and we know that's specifically an Aetna member.
And that's beneficial because when you're a pharmacist, if you're a pure play pharmacy, you don't necessarily have all this other ecosystem of relevant background medical information, you just have specifically what you have in the system for their drugs. But when you're an Aetna member, there's all this other stuff.
And these are things by the way, these are still very early stage, our companies have merged in the past two to three years, but that is live and active in some types of behavior changes now. And we're in the process of expanding, testing, rolling out.
And it's tricky because you also, there are certain things that may be less appropriate for a pharmacist to talk about. So, we have to make that balance very clear. There's privacy implications, too. So this is something that's being treaded carefully but it's certainly an opportunity.
Lygeia:
Absolutely. That makes sense. And then would the pharmacist have an opportunity to give feedback to others within the broader Aetna system, too
Rahul:
Yeah. It's a two-way feedback loop and we're close with our folks in the retail pharmacy organization, and it's a partnership to build a program like this and basically create a proper integrated system for continuity of care.
How is continuity of care ensured across health care providers through technology? (11:31)
Lygeia:
Yeah. I can imagine that the, that's what I was going to ask you about next actually. This continuity and how you manage to pull all these pieces together and keep it all updated. Do you sort of presume that many of the members are going to be using an app primarily, or is that not necessarily even part of the picture?
Rahul:
Yeah, it’s part of the picture. It’s probably the most ideal scalable interface because we don't pay money to put a message there. You don't have to pay postage, you don't have to pay Google or Facebook a fee to put a message out there.
I think that and pharmacists, the pharmacists, are also not necessarily scalable if it's only at a certain point in time when you're physically there, and not everybody actively has a drug with our pharmacy systems.
So absolutely, a mobile app is a great platform for that. It doesn't have to be the mobile app. It could be just logging into our, the web version of our authenticated sites. So all of those things are great. We recognize it's not a large percentage of people yet. So until then, there's a lot of coordination with all these other channels I mentioned.
How personalized are these automated “nudges” for members? (12:48)
Lygeia:
Gotcha. I'm curious about, you've talked about how information and data from numerous sources can help you to kind of target the kinds of information that are appropriate for people. Are you also able to, in terms of the nudging aspect, do you also personalize in terms of like this person prefers to hear things through text or they prefer a particular tone?
How much down that road of personalization are you going, or is the personalization mostly about sort of the medical and predictive qualities of what someone might need? Or does it get into it at all like, well, this person prefers to have messages in a certain way?
Rahul:
Yeah. So there's different layers of personalization here. Let me talk about a couple of them. So, one layer is around targeting. And so I've already talked about that, and we'll use machine learning to suggest maybe there's a higher probability that a message is going to be relevant to you. So that's one level of personalization.
If you're getting the message, you can still personalize to groups. So we're not at one-to-one yet, but let's talk about that and kind of like go down the funnel. So at the group level, for example, let me give you an example with mammograms. If you're trying to reach Medicare women and a stat is in our population, it might be that around 30% of them are not getting mammograms when they should be on some regular cadence.
So you could reach out to a cohort that is maybe not getting it because they're managing too many chronic conditions and they're not thinking about preventative screenings. And that's different than a cohort that is physically too far from an actual screening clinic.
And you can just as easily imagine how those two cohorts, the messaging is automatically different for that. And you can very easily think about as a marketer, or even just as a human, how do you talk to those women differently? So that's like kind of cohort level.
And then there's the level of one-to-one personalization which is going to be based on their specific health condition. And as much as possible, we will try to maximize personalization on all these layers. You have to be limited to privacy compliance channels such as enveloped mail or being logged into an app once you get that specific where you've referenced someone's condition.
And you asked about preferences, preferences are interesting. We're not actively told if someone preferences these channels. The main thing is, are you permissioned into certain channels? And so those will be acknowledged. But what I'll tell you about preferences and what's working is that multi-channel touch points are most effective at successfully driving changes to health behavior. Any marketer would probably tell you that makes sense.
And there's a certain level of predictability you have to say that somebody who is already actively using certain digital channels, whether it's email or mobile app, they're probably already on their own kind of a person who's actively managing their health because they're also likewise choosing to get messages from their health insurer or their provider.
They're intrinsically more engaged with their health than that. So I'm not saying it's causative there, but there's a strong correlation with people who just opted into permissions.
How is behavior change using AI in health care measured? (16:21)
Lygeia:
That makes sense. You've talked about sort of efficacy levels and I'm wondering, I know you mentioned that this is all still relatively early stage. But have you been able to actually measure the kind of actual impact in terms of changing behaviors? Is that the kind of thing that you have yet?
Rahul:
Yeah. We've been running this program for years now, and it's evolving and increasingly having a larger portfolio of behavior change opportunities. So we use a mix of metrics.
Chief among them would be health outcomes data, there's also medical cost savings that you can measure through claims data. It could be as simple as just like the, how many more people are getting colon cancer screenings, or how many women are getting mammograms?
There's also a famous set of standard measures called HEDIS, which is the Healthcare Effectiveness Data Information Set, which you know about. And so there's all these different metrics we could use. I think the one thing I'll say about measurement is, everything we do is measured against randomized controlled trials. And it's the same methodology you use to ensure there's statistical significance that you would see in clinical trials for a new drug. So it's the same methodology.
And that’s because what we're trying to do is measure incrementally about how much better are we performing on these behavior change interventions compared to a holdout or compared to different types of treatments or messages, maybe using different behavioral economics principles infused in the language we use, things like that. So we're always trying to optimize.
What are the biggest barriers to health behavior change from your perspective? (17:56)
Lygeia:
Very cool. What would you say just from your experience thus far, what are some of the biggest barriers that you're encountering to change? Whether it's in the daily health and wellness sphere or in more of the sort of navigating the healthcare system. What tend to be the ones that would have the biggest impact if you could make them go away?
Rahul:
Yeah. It's one of those things where I want to take an easy way out and say it really depends on what the behavior change objective is and what population type you're talking about. And for a lot of people, it can be the cost, their out of pocket costs.
For a lot of people unfortunately, it's just simply access to the care. Do you even live in an area with access to primary care doctors that can guide you towards more preventative outcomes? And so, it does depend on the population, but those are some big barriers I mentioned, cost and access.
There is another massive barrier, which is just simply not knowing any better. And this is sort of like we're trying to bridge the gap in education where there are automatic processes in a system that can artificially lock or make you think you're locked into certain things that are decided for you.
So, even simple things that you get a referral from a provider to go to a certain type of option for care or a certain place for your procedure, but you may not be aware that your area has other in-network same-day procedural centers that can help you do this exact same procedure for a lower cost and lower infection rates than a hospital.
So just like, that kind of nuance about where the places I can go. The nuance's necessarily worth sharing... And not everybody knows they have the power to choose or that they have the power to talk to their doctor about what their options are, and some may not even know what's in their network. So, that's where the plan can sort of jump in and say, this is what makes, these are the options you have.
Lygeia:
So, I'm just imagining for a second that I go to my doctor and she says, I'd like you to get an XYZ test. Here's a place to go get it. And then maybe might this play out that sort of I go home and I get an email or a text or maybe even a call or whatever from Aetna because they'll know on the other side that my doctor wants me to do this test and might suggest to me like, hey, why don't you try the place down the street available sooner at a lower cost to you or to us or both.
Rahul:
Yep. That's exactly right. And like those kinds of messages that we might send on any number of channels could be triggered based on the actual data we're getting from the provider. They could be predictive based on what we think someone may be getting or what they may be talking to their doctor about.
So it can get into all sorts of different levels. And a lot of it may not work, which is why it's all about just testing and learning and seeing what things make sense for these types of things. Whether it's labs or procedures or what have you.
Can consumers opt-in for these reminders and personalized messages? (21:13)
Lygeia:
So, my next question is very much from the perspective of consumers and myself as an actual consumer. So let's say I'm super excited about your program, which I am, and I'm thinking, hey, I wanna be a part of this, not only because I think this sounds like a great thing for health care in general, but also, hey, I could use some nudges in making either my health and wellness optimized.
Or my goodness, I want to be absolutely sure I don't miss it next time when there is another facility I could go to down the street that would be better. Is there anything that a member can do to kind of opt in and or signal like super engaged readiness?
Rahul:
Yep. And I will tell you the problem. I'll start with one of the annoying things for a consumer to hear where it depends on your plan. And the reality is we're still in the early years of scaling up our program, and what I've described to you is not necessarily available to everyone. It does depend on your employer or what your group sponsors selected for you. It's at scale for our fully insured population for example and government plans.
But one thing that I can say to play it safe, regardless who you're covered by or what plan you have, go to your health plan website and make sure they have your email address, phone number, make sure you're registered for their app and use it. And look, this is totally different than like a Starbucks or Best Buy trying to get you into their ecosystem of their daily emails or their app.
Remember, health insurance companies are aligned to consumers in the sense that we are also likewise buyers of healthcare. So insurance companies are able to do better on behalf of their members and help them keep them healthier and drive more cost-effective decisions if you can treat the plan as a partner.
And my short answer is, just make sure that your partner can send you messages back. So, whether it's like Aetna, if you're an Aetna member or if you are in any other health plans, because these are the kinds of things I'm describing that many health plans are trying to get into at different levels of effectiveness, that is probably the best way to do it.
The status of Aetna’s partnership with Apple using smartwatches (23:38)
Lygeia:
Cool. You mentioned earlier that you have a partnership with Apple, Apple watch. And I actually, I was at a launch event for that program. What was it, a year and a half ago or something? So I'm really curious, where is it now? Is it available? I assume primarily via employer plans, is it also through some public plans? Where is it?
Rahul:
It's a good question. I don't know exactly which plans, but it is not all plans. And for folks who don't know the program, it's called Attain by Aetna and it's a rewards-based program that's encouraging people to achieve their health goals and offering personalized goals and just earning points and earning and burning them. And you can get rewards for staying healthy.
So that's how it works. It is dependent on certain health plans that we're a part of. But it's something we're excited about, we hope to scale it more. Again, it's another place where we can sort of encourage sort of the types of behaviors that will keep people healthier and overall reduce the cost of, the medical cost burden in our entire system.
The prevalence of behavior-nudging mechanisms & the future of AI in health care overall (24:56)
Lygeia:
So, very cool. To go back to this question again of how this might apply to listeners who might not be Aetna members. Do you have a sense of the extent to which it is? Are you guys like, way out in front relative to many of the other insurers in terms of experimenting with this kind of behavior-nudging mechanisms, or do you guys think a lot of different folks are trying it?
How much should people be expecting to, they might not even be aware of it necessarily unless they hear something like this or read about it, because it may just flow into their lives. But is this going to be commonplace in a few years, do you think, or where is it in terms of adoption and growth?
Rahul:
Yeah. I think it is definitely the future for many, and you can look at any companies talking about how can we use AI to do what we do better, either more efficiently, or just more effectively? For certain, I could say our methods of AI-driven behavior change are being used at some other insurance plans.
But they're not being widely used given the expense of being associated with hiring data scientists, data engineers and, you know, marketing technology capabilities. You need to automate these types of scalable member journeys. So certainly I could say it's not pervasive, and there are probably a handful of plans that are doing this. That would be my take on it.
The effectiveness, and look, I gave you some examples at the beginning like, educating people to go to urgent cares or retail clinics instead of an ER if you don't need to. That is a basic program that's existed for many, many years.
The question is, how targeted is the message, and how evolved is that program to educate people on a journey? And then how are you doing so in a way that's relevant for the message? And would you get that message when it matters? And as a consumer, you can remember that tip. That's where it gets down to.
So I think everybody is, all health insurance companies have different things that they are educating members on. I think the question is, one, how effective is it? And two, how deep does the well go with different types of behavior change programs? Because as you get deeper, you're getting to really clinical things that are very difficult to message, and certainly you can't message that on a mass basis. You have to be targeted, you have to be relevant.
And I think the third thing I'd say to that is, how integrated is your health plan with other provider networks? That you can have things such as accountable care organizations that have shared incentives with the provider system which is based on... Aetna of course plays in. You talked about the partnership with CVS and Aetna. You have that continuity of care of 10,000 pharmacies and 1,500 health hub locations which have minute clinics to get actual care through a nurse.
So you have all these other elements that can layer in, but not all health plans will necessarily have that. So I think you're just going to see different implementations and different levels of effectiveness. Hopefully that answered your question on that.
How is Aetna sharing its learnings on behavior change marketing? (28:21)
Lygeia:
Gotcha. Yeah. I was curious too, I think I read something about the possibility that you guys at Aetna may be considering longer term I guess taking some of these approaches and potentially sharing them with other plans or employers, and sort of making the expertise that you're gaining now available to others. Is that something you guys are thinking about?
Rahul:
It is. And so, we've already done it. We've productized, as they say, this behavior change capability and we call it "health advisor". It's something that we're currently selling to other health plans that contract with Caremark as their pharmacy benefit manager or PBM. And that launched at the beginning of this calendar year. So, we've been working on it for the past year, and are very excited about that.
We're going to be growing that capability and building that portfolio of behavior change nudges that are available to other plans. Likewise, those behavior change capabilities are being packaged into very condition specific solutions such as diabetes management. And that again is sort of a program that's been active and we've been selling that to, in a payer agnostic fashion to other health plans, too, for some time now.
What’s on the horizon for Aetna-CVS and what are you excited about? (29:40)
Lygeia:
Very interesting. What else is on your horizon? What are you excited about developing further in the year even plus going forward?
Rahul:
Yeah. It's continuing to grow the program by testing and learning and improving the effectiveness of current behavior change nudges. We have a much longer list of nudges that are still in pilot mode. So if we get it right, we're going to continue to scale that and just get better.
From a capability standpoint, I've mentioned how I am excited about continuing to integrate more with our retail footprint. So, many clinics and health hubs to provide options for care, particularly for chronic populations. So as soon as we, we're going to continue to activate those capabilities.
And also very exciting is Aetna is reentering the ACA exchanges for individual plans at the beginning of 2022. So we are excited about extending the same capability to that population as well.
Lygeia:
Very cool. Any other key points about the program or your work that we might've missed that you wanna share particularly with the consumer audience?
Rahul:
I think that's the main thing. I will say there's so much, just thinking off the cuff, I think there's a lot of passion to help fix healthcare. Everyone in our world, in my world within Aetna and then sort of the broader CVS health enterprise, we're so conscious also as consumers of healthcare that it's so difficult to navigate care, it's so difficult to pay for care.
And I think that especially in the last year, healthcare is just top of mind for everybody in the world. And I think that it's just so, I consider myself really lucky to have made the choice to be here. And not necessarily in this company, too, but just like, being in healthcare.
I didn't think I'd be as passionate about it as I've sort of found, especially in the past couple years, and that this is something I'm excited to stick with and hopefully make better, and a lot of my colleagues feel the same way.
How do Rideshare services come into play to address the access to health care? (31:57)
Lygeia:
You know, you did, as you were speaking, you reminded me of another question I had which was, you talked about a barrier to care being, for many people, just access to care. So it's that simple, how do I get across town and that kind of thing.
I know that some folks in the healthcare universe are doing things like subsidizing or partnering with rideshare services and things like that. Is that something, are you guys employing those kinds of ways to address the access challenge?
Rahul:
Yeah. That's something we offer for example, some of our Medicare plans. So that category by the way in the industry is called "non-emergency medical transport." And so, there are partnerships with rideshare companies to offer that as a capability.
We also, we've done pilots where we've tested it for very specific conditions and very specific populations where we think there may be sort of access issues there. So, it is one of the tools in our behavior change toolbox.
Lygeia:
Excellent. Good to hear. I was curious about that as you were talking about it.
Well, I wanna thank you just so much for taking your time and explaining what you guys are doing at Aetna-CVS. I appreciate it greatly. Again, I think it has ramifications for the whole industry, both because you guys are such a big player and because I just, it feels like this is a general direction that the industry seems to be moving in. So I appreciate your shedding some light on it.
And I want to encourage those of you who are listening, thank you so much for tuning in. I want to encourage you to sign up for our YouTube channel and to subscribe to AdaRose on Instagram and also to weigh in and share what you are interested in.
What kinds of health and healthcare challenges are you confronting that you're most interested in? And what you would love to hear about from experts like Rahul who can help to illuminate the future and shape it, even co-design it?
So, thank you so much. And until next time, see you later!
Rahul:
Thank you, Lygeia.